More than 50,000 children, adolescents, and young adults under age 20 in the U.S. are living with or in remission from leukemia, lymphoma, myeloma, and other related syndromes, according to the Leukemia & Lymphoma Society. That number is greater than all undergraduate and graduate students at the University of Washington.
About 10,000 of those children’s cancers are myeloid in origin. They represent a spectrum of blood or plasma-related malignancies; most are acute. Many of the parents and caregivers of these children find hope in the five-year survival rates of acute myeloid leukemia (AML), a cancer of the blood and bone marrow. Statistics from the National Cancer Institute indicate the rates are 68% for children younger than 15 and 57% for adolescents ages 15 to 19.
But for BBI’s Dr. Scott Furlan those percentages represent “unacceptably high mortality rates.”
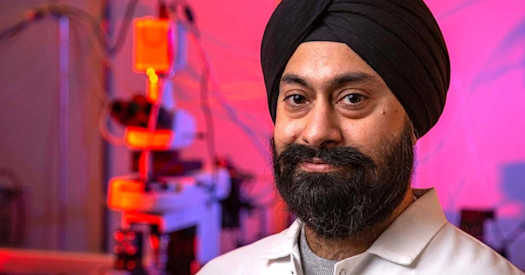
Furlan is a physician-scientist who serves as an Assistant Professor at the Fred Hutchinson Cancer Research Center and in the Department of Pediatrics at the UW. He is the Lead Principal Investigator of a $150,000 BBI grant, awarded in January of this year, measure residual disease and to predict more accurately the cancer’s relapse. Others participating in the grant are Todd Cooper, a Pediatric Hematologist at Seattle Children’s Hospital, and Clinical Researchers Soheil Meshinchi and Sami Kanaan at the Fred Hutch.
“Our team of researchers believes that leukemic ‘stem’ cells are a critical component of pediatric AML,” Furlan said. “We’re seeking to rigorously quantify these leukemia initiating cells in patients with residual disease by using leading edge, single-cell analysis. Moreover, we’re hoping our experiments will form the foundation for an entirely novel approach to measuring residual cancer cells that, in turn, will more accurately predict relapse than current conventional approaches.”
The project is two-fold:
- Assessing retrospectively the feasibility and predictability of residual leukemia by analyzing extensively annotated clinical data in biorepository of 50 children from throughout the U.S., with a particular emphasis on biomarkers corresponding to leukemic relapse.
- Comparing prospectively the profiles of residual disease at 28 days to the time of diagnosis across 30 patients being treated at Seattle Children’s Hospital.
“This study, which we expect will take about two years, is certainly pretty novel,” said Furlan. “We need of proof-of-principle data that single cell genomics will be able to potentially deliver more information and more confidence in assessing the potential – or even likelihood – of children relapsing.”
The project, entitled “Needles in the Haystack: Genomic Signatures of Residual Leukemia at Single Cell Resolution,” is one of 17 funded in 2022 by BBI, among more than 32 applications. Total amount was $1.7 million. in 2022.
This was BBI’s fourth annual grant program awarding funds to researchers at all three of its member organizations – UW Medicine, the Fred Hutchinson Cancer Research Center, and Seattle Children’s. Of the two award categories, 14 were awarded through Catalytic Collaborations, and three through Precision Medicine Clinical Labs. For more information on the awards and a complete list of 2022 recipients, visit https://brotmanbaty.org/grant-program
“Our team is very appreciative of BBI for this grant,” said Furlan. “We will learn a lot and this study has the potential to be groundbreaking. I have a lot of hope for this technology and the ability, ultimately, to better inform clinical treatment.”